Melanoma of the skin is the most serious of the three common types of skin cancer.
Melanoma Diagnosis and Treatment in New Zealand
The Quality Statements to Guide Melanoma Diagnosis and Treatment in New Zealand are now available on the MelNet website.
This document has been developed by the National Melanoma Working Group, with support from MelNet and Te Aho o Te Kahu - Cancer Control Agency.
The statements describe what quality care for melanoma should look like in New Zealand and will help inform efforts to reduce the incidence and improve outcomes for melanoma patients and their families.
The formal launch took place at the virtual 2022 New Zealand Melanoma Summit in February 2022. MelNet will endeavour to ensure the document is updated regularly to reflect the latest evidence. Reviews will be held twice yearly.
What is melanoma?
Melanoma is a cancer of skin cells called melanocytes. Melanocyte cells make the dark-coloured pigment called melanin, which gives the skin its colour.
Melanoma skin cancer begins when these melanocyte cells begin to grow and spread abnormally.
Cancer is a disease of the body's cells. It starts in our genes. Our bodies are constantly making new cells, a process controlled by certain genes. Cancers are caused by damage to these genes. As the damaged cells replicate a lump or tumour is formed.
Tumours can be:
- Benign - not cancerous. These do not spread to other parts of the body.
- Malignant - cancerous
These cells are found in many other parts of your body, including the eye, hair, and lining of the internal organs.
Rare melanomas can occur in other parts of your body or on the skin that has never been exposed to the sun. These include:
- The eye (ocular melanoma)
- The mouth, gastrointestinal tract (gut), vulva, vagina, or anus (mucosal melanoma)
- Under fingernails or toenails (subungual melanoma)
What does melanoma look like?
The first signs of melanoma are usually changes in your skin.
Melanoma often starts as a new spot on your skin, but a mole you already have can turn into melanoma.
Look out for changes in:
Size
A spot or mole may get bigger.
Shape
A spot or mole may have an irregular, not-smooth edge or surface.
Colour
A spot or mole may change colour such as brown, black, blue, red, pink, white and/or light grey.
Thickness
A spot may become raised over time.
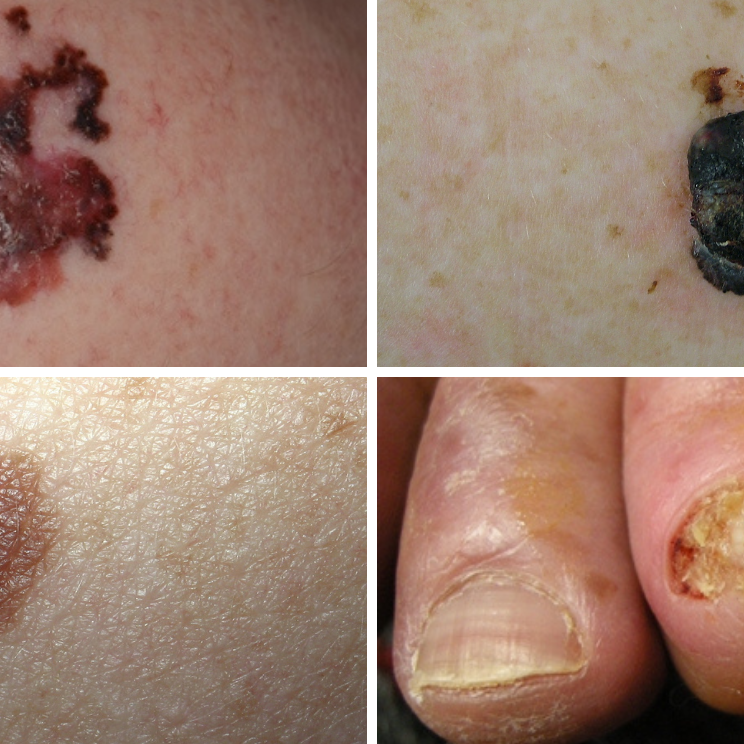
Melanoma has many different sizes, shapes and colours. Any change on your skin should be checked by a doctor.
If found early, melanoma can usually be completely removed by surgery.
Tips for talking to your doctor
- make a list of what you are feeling and how often it happens, including as much detail as possible
- think about your family/whānau history of cancer and tell your doctor
- go back to your doctor if you don't feel better, even if tests show you don't have a problem - you can ask for a second opinion if you want one
- take a family/whānau member or friend with you to the appointment for support
What causes melanoma?
Melanoma is most commonly caused by skin cells damaged by ultraviolet (UV) radiation from the sun.
People of all ages and skin colours can get skin cancer, but those at higher risk have:
- had skin cancer before
- family/whānau members with skin cancer
- a skin type that sunburns easily
- red, blonde or light-coloured hair
- many moles or larger moles
- used sunbeds/tanning beds (solariums)
- spent a lot of time in the sun unprotected

Doctors will check the changes on your skin and order more tests if needed.

Treatment of melanoma depends on how far it has spread in your body.

Learn how to be SunSmart by enjoying the sun safely.

Skin cancers are one of the most common cancers in NZ. Recognition of early signs and early seeking …
We know that going through cancer is tough and can raise many questions. You are not alone.
We have health professionals to answer your questions and provide the support you need.
Get in touch
