If you've been diagnosed with breast cancer, knowing the stage of the cancer will help your treatment team give the best treatment options for you.
What are the stages of breast cancer?
The breast cancer stage tells you the cancer's size and whether it has spread to other parts of your body.
Based on your test results, the treatment team will give the cancer a stage between 0 to 4.
In general, the higher the number, the more the breast cancer has spread in your body.
| Stage | Definition | |
| Stage 0 | Ductal carcinoma in situ (DCIS) | A non-invasive pre-cancerous change |
| Stage 1 | The cancer is only found in your breast with no or only microscopic involvement of lymph nodes in your armpit. | Early breast cancer |
| Stage 2 | The cancer is larger than in stage 1 and/or is found in just a few nearby lymph nodes. | Early breast cancer |
| Stage 3 | The cancer is larger than in stage 2, or involves the skin of the breast or the chest wall, or is a type of breast cancer called inflammatory breast cancer, and/or has spread from the breast to more than just a few lymph nodes close to the breast. | Locally advanced breast cancer |
| Stage 4 | The cancer has spread to other parts of your body. | Advanced breast cancer |
Lymph nodes (also known as glands) are found throughout the body and are part of the lymphatic system.
The lymphatic system contains a series of lymph vessels (tiny channels under the skin) that carry the lymph fluid through the nodes back to the bloodstream.
Lymph nodes contain white blood cells that help fight infection and diseases, such as cancer.
The number of lymph nodes you have is different for each person.
For example, there can be between 15 to 30 nodes in an armpit. Lymph nodes also vary in size from a pinpoint to the size of a baked bean.
Lymph nodes can swell and become tender when you have an infection. If you develop a swollen lymph node, get it checked by your doctor.
Sometimes, cancer cells spread into the lymph nodes from cancer in another part of the body. It is also possible for cancer to start in a lymph node. This type of cancer is called lymphoma.


What are the grades of breast cancer?
The grade of the cancer describes what the cancer cells look like compared to normal cells.
This tells the treatment team how quickly the cancer is growing and the risk that it may spread to other parts of your body.
| Grade | Definition |
|
Grade 1 (Low grade) |
Usually slow-growing, the cancer cells and structures look more like normal breast cells |
|
Grade 2 (Intermediate grade) |
Intermediate growth rate, the cancer has fewer features of normal breast tissue |
|
Grade 3 (High grade) |
fast-growing the cancer cells look very different from normal breast cells |
What would you tell a friend who was expecting a cancer diagnosis?
We asked Lucy to tell us what she wished she'd known before being diagnosed with breast cancer.
After a diagnosis
If your test results show cancer, this can be a difficult time, and feelings can change from one moment to the next.
Everyone reacts differently when they learn they have cancer. There is no right or wrong way to feel.
Talk about your treatment options with your doctor, family and friends. Ask for as much information as you need. It is up to you how involved you want to be in decisions about your treatment.
Prognosis for breast cancer
The prognosis is the likely outcome of a disease.
If the test results show breast cancer, you may wish to speak with your treatment team about the prognosis.
The doctors will look at the type and stage of the cancer as well as your age and general health to give a prognosis, but no doctor can predict the exact outcome for you.

Breast cancer forms in the cells of the breast tissue. It can occur in women and, rarely, in men.

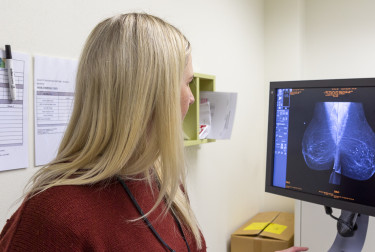
Breast cancer is diagnosed using a mammogram, ultrasound, MRI scan and biopsy.

We've put together a list of questions you may wish to ask your treatment team.
Breast cancer can be treated by surgery, radiation treatment, chemotherapy, hormonal therapy, and ta…
We know that going through cancer is tough and can raise many questions. You are not alone.
We have health professionals to answer your questions and provide the support you need.
Get in touch
